Subcutaneous vs Intramuscular Injections: Which Is Really Better for You?
When people compare subcutaneous (SC) and intramuscular (IM) injections, they often focus on speed or pain, but patient experience tells a bigger story: in some large cancer datasets, 92% of patients preferred subcutaneous therapy over other routes because it was faster and less disruptive to daily life. As a team focused on testosterone replacement therapy (TRT) tracking and education, we see the same questions every week: is subcutaneous or intramuscular better, safer, less painful, and more consistent?
In this guide, we break down the evidence in a practical way, so you can understand the trade-offs and have a more informed discussion with your healthcare provider about how you inject medications like testosterone, biologics, vaccines, or pain medications.
Key Takeaways
| Question | Answer (What the Evidence Suggests) |
|---|---|
| Is subcutaneous or intramuscular better overall? | Neither route is “best” for everything. Subcutaneous is usually better for chronic, self-administered therapy (comfort, convenience, long-term adherence), while intramuscular can be better where faster absorption or specific immunogenicity is needed (e.g., some vaccines). |
| Which route do patients usually prefer? | Across multiple chronic conditions, most patients prefer subcutaneous injections at home. For example, a large cancer-focused study found 92% of patients preferred SC therapy due to convenience and shorter visit time. |
| Is SC as effective as IM for long-term therapies? | For many biologics and analgesics, SC has been shown to be non-inferior or even superior to IV/IM on key outcomes. The specific drug matters, but for things like infliximab in IBD, SC can actually rank first across several endpoints. |
| What about testosterone injections? | TRT is commonly prescribed IM, but many clinicians now allow SC dosing off-label. We built our Himcules platform because tracking dose, route, and labs over time is essential when changing from IM to SC. |
| Is one route safer than the other? | Both are generally safe when done correctly. IM can carry higher risk of nerve or vessel injury if technique is poor; SC can cause more local lumps or irritation for some drugs. For influenza vaccines in some Japanese data, IM actually had fewer local adverse events than SC. |
| How should I decide which route is right for me? | Decisions should be made with your prescriber, balancing drug-specific evidence, your body composition, needle comfort, and your ability to self-inject. If you have complex questions, you can always reach out via our contact page so we can point you to relevant educational resources. |
| Where can I learn more about our approach? | We explain our TRT tracking philosophy and why we care so much about route of administration in our About this site section and on our blog, where we publish practical guides for injection users. |
Understanding Subcutaneous vs Intramuscular: What Actually Differs?
Before asking whether subcutaneous or intramuscular is better, we need to be precise about what each route actually does. The difference is not just “deeper needle vs shallower needle”; it changes how the drug moves through your body and how you experience the injection.
What Is a Subcutaneous Injection?
A subcutaneous injection delivers the medication into the fatty tissue just beneath the skin. This layer has fewer blood vessels than muscle, so absorption is slower and smoother in many cases. People often use short, fine needles and inject into the abdomen, thigh, or upper arm.
Because the technique is easier to learn and less intimidating, subcutaneous injections are commonly used for insulin, GLP‑1 agonists, many biologics, and increasingly, off‑label TRT in some practices.
What Is an Intramuscular Injection?
An intramuscular injection delivers medication directly into the muscle, which has a richer blood supply. That usually allows faster and sometimes more complete absorption for certain drugs, especially vaccines and oil-based hormones like testosterone.
IM injections often require longer needles and careful landmarking (e.g., ventrogluteal, dorsogluteal, or deltoid sites) to avoid nerves and blood vessels. The technique is more demanding, and pain or soreness after injection can be greater than with SC for many people.
How Absorption and Effectiveness Compare: SC vs IM
When we ask “Is subcutaneous or intramuscular better?”, we are usually asking about drug levels and clinical outcomes. The answer depends heavily on what is being injected. Still, we can map some general patterns across drug types.
Biologics and Chronic Injections
For biologic drugs used in autoimmune conditions, real-world and trial data now show that subcutaneous formulations can match or outperform IV/IM options in some outcomes. In inflammatory bowel disease, a network meta-analysis of 2,519 patients found subcutaneous infliximab often ranked first versus IV on multiple disease control measures.
Another analysis reported strong or very strong evidence that SC infliximab was superior to IV for clinical remission at 30 and 54 weeks, with similar endoscopic outcomes by week 54. In other words, for some biologics, SC is not just more convenient—it can perform at least as well clinically.
Pain Management and Analgesia
A systematic review of analgesia routes found that subcutaneous administration can be non-inferior to IM/IV for cancer and postoperative pain control. Route‑related adverse effects were rare across methods, suggesting SC is a viable option when trained staff or IV access are limited.
From our perspective, this matters because it supports a broader principle: if the drug’s pharmacology allows it, subcutaneous can often maintain efficacy while offering easier, more flexible delivery.
Patient Preference: Why Subcutaneous Often Wins
If we only looked at pharmacology, we would miss the real world. Patients live with injections week after week, and their preferences tell us a lot about what works long term. Across conditions, subcutaneous administration usually comes out ahead when the drug is the same.
Chronic Diseases and Home-Based Care
In combined real-world datasets for primary immunodeficiency and autoimmune diseases, about 80–83% of patients preferred SC administration over alternative routes when they had the choice. Quality-of-life metrics and satisfaction were often higher when patients could inject themselves at home.
In a large US oncology study, 92% of cancer patients preferred subcutaneous therapy over IV, with 80% calling it more convenient. Many highlighted that SC visits were faster and less disruptive to work and family obligations.
Experience Changes Preference
In inflammatory bowel disease cohorts, many patients initially resisted switching from IV to SC formulations. But when people had experience with both routes, a large share began to prefer more frequent SC injections (e.g., every 2 weeks) over less frequent IV infusions (e.g., every 8 weeks) once they understood the trade‑offs.
This fits what we see with TRT users: early on, the idea of injecting yourself more frequently can sound worse, but after a few months of easier, smaller SC injections, many users report they would not go back to deep intramuscular dosing if they can avoid it.
Safety and Side Effects: SC vs IM in Practice
Safety is central when we ask if subcutaneous or intramuscular is better. Both methods are widely used and generally safe when done correctly, but their risk profiles differ in important ways.
Local Reactions and Injection Site Issues
Subcutaneous injections more often cause small, localized reactions: redness, mild swelling, or nodules under the skin. These are usually temporary but can be annoying if injections are frequent or volumes are high.
Intramuscular injections can cause deeper muscle soreness, hematomas (bruises), and—in rare cases—nerve or vessel injury if the landmarking is incorrect. For people with less muscle mass or higher body fat, consistent IM technique can be challenging without professional help.
Vaccines: A Case Where IM Can Be Better
Not all drugs behave the same. For example, in a Japanese dataset on influenza vaccines, intramuscular vaccination was associated with fewer local adverse events (8.2% vs 11.3% for SC) and better immunogenicity than subcutaneous vaccination.
That matters because it reminds us not to overgeneralize: for some vaccines and specific formulations, IM is not only the recommended route—it may give better immune responses and fewer injection site problems than SC.
Testosterone Replacement Therapy (TRT): SC vs IM in the Real World
Because our platform focuses on TRT tracking, we pay special attention to how route affects testosterone users. Historically, guidelines have favored intramuscular injections (e.g., testosterone cypionate or enanthate in the glute or thigh), but practice has evolved.
Why Many TRT Patients Ask About SC
TRT users often self-inject weekly or even multiple times per week. Over time, that makes needle comfort and technique a major quality-of-life issue. Subcutaneous injections with smaller needles into the abdomen or thigh can feel less intimidating and less painful, especially for lean individuals or those nervous about needles.
Some clinicians now prescribe or allow SC TRT off‑label, particularly at divided doses. While large, formal head‑to‑head trials are limited, many case series and clinic experiences suggest stable testosterone levels and high patient satisfaction with SC protocols when dosing is adjusted.
Why Tracking Matters When Changing Routes
Changing from IM to SC often means changing dose, frequency, and expectations. That’s exactly why we built our Himcules tracking tools—to help users log route, site, dose, and lab results over time, then discuss the patterns with their clinician.
We always emphasize that TRT dosing and route decisions must stay within a medical treatment plan. Our role is to provide structure and visibility so that patients and prescribers can see, rather than guess, how a route change is affecting symptoms and bloodwork.
Technique, Needle Size, and Comfort: Practical Differences
Route is not just about where the drug ends up. It also changes how you inject, what equipment you use, and how confident you feel doing it yourself. These details can decide whether SC or IM is “better” in day‑to‑day life.
Needle Length and Gauge
- Subcutaneous: Often uses short (4–12 mm), fine needles (28–31G) similar to insulin or GLP‑1 pens. These are typically less painful and easier for self‑administration.
- Intramuscular: Commonly uses longer needles (25–38 mm or more), with gauges around 21–25G, depending on viscosity and site. These can feel more intimidating, especially for new users.
For many TRT and biologic patients, this difference alone makes SC feel like a more approachable, sustainable option when it is medically acceptable.
Learning Curve and Consistency
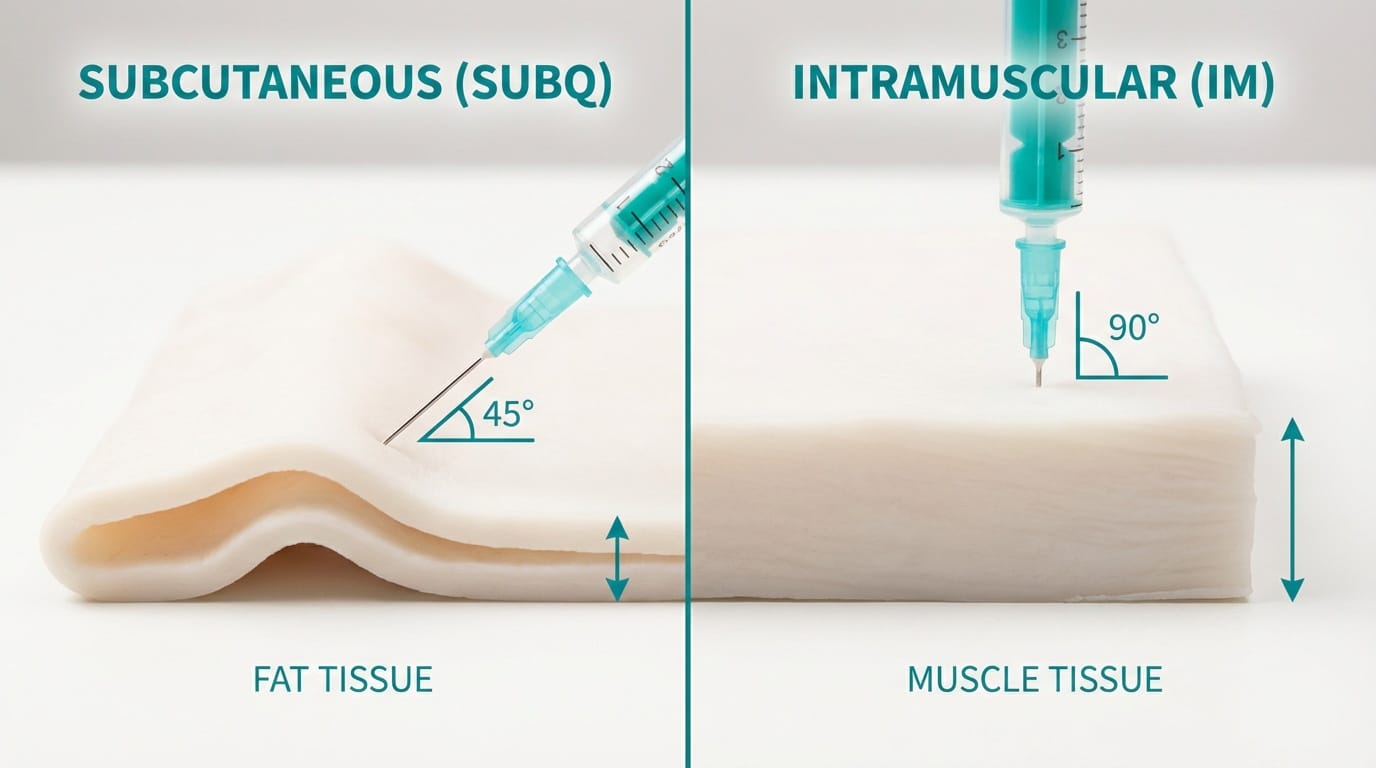
We find that patients usually reach consistent technique faster with SC injections. Pinching a skin fold and inserting a small needle at 45–90 degrees is simpler than finding the correct muscle landmarks and depth for IM.
Consistent technique matters because inconsistent depth (especially in IM injections in overweight or very lean individuals) can unintentionally turn some doses into partial SC injections. That blurs the line between routes and can make drug levels less predictable.
Condition-by-Condition: When SC or IM Is Usually Better
To move from theory to practice, it helps to look at common conditions where both SC and IM (or IV) are options. The table below summarizes general trends based on current evidence; your individual plan may differ.
| Condition / Therapy | Typical Preferred Route | Why This Route Often Wins |
|---|---|---|
| Inflammatory bowel disease (infliximab) | Subcutaneous (after induction) | SC can match or outperform IV on remission rates, higher convenience, home dosing. |
| Primary immunodeficiency / autoimmune biologics | Subcutaneous | Strong patient preference (≈80%+), at‑home use, similar efficacy. |
| Cancer supportive/targeted therapies (where dual routes exist) | Subcutaneous | 92% of patients in some cohorts prefer SC; visits are shorter and less disruptive. |
| Influenza vaccination (some Japanese data) | Intramuscular | Lower local adverse events and better immunogenicity vs SC in specific studies. |
| Pain management (cancer, post‑op analgesia) | Subcutaneous or IV/IM depending on context | SC shown non‑inferior in many settings and can be simpler when IV is not practical. |
| Testosterone replacement therapy | Intramuscular (traditional) or Subcutaneous (emerging) | IM is on‑label standard; SC offers easier self‑injection and is increasingly used off‑label in some practices. |
Long-Term Adherence: What Keeps People on Therapy?
In chronic conditions, the “best” route is often the one a person can actually stick with for years. Missed doses, skipped injections, or clinic fatigue can quietly undermine otherwise excellent treatment plans.
How Convenience Drives Adherence
Data across autoimmune, immunodeficiency, and oncology care consistently show that when subcutaneous administration offers equivalent outcomes, patients prefer it—often by a large margin. That preference translates into better adherence because it is easier to fit SC dosing into everyday life.
When patients can inject at home, they avoid travel time, time off work, and the stress of frequent hospital visits. In oncology studies, most SC visits finish in under an hour, while IV infusions often take much longer, further pushing patients toward SC where possible.
Psychological Comfort and Sense of Control
We also see a psychological layer: patients who learn to self‑inject via SC often report a stronger sense of control over their treatment. That sense of ownership can increase engagement with tracking tools, lab follow‑ups, and dose discussions with their clinicians.
In contrast, deep intramuscular injections can keep some patients dependent on clinic visits or anxious about self‑administration, which can become a barrier over the long term if not addressed.
How to Decide With Your Clinician: A Practical Checklist
We never recommend changing your injection route on your own. However, we do encourage you to have a structured conversation with your prescriber using a simple checklist.
Questions to Ask About SC vs IM
- Is this drug approved or at least well‑studied for subcutaneous use? Some medications must be IM for safety or effectiveness.
- What are the expected differences in absorption and side effects? Ask about how peak levels, trough levels, and common reactions change by route.
- Can we adjust dose or frequency if we switch routes? Small, frequent SC doses may need different scheduling than less frequent IM doses.
- How will we monitor the change? Plan lab timing, symptom tracking, and follow‑up visits in advance.
Using Tracking Tools to Support the Decision
For TRT specifically, we designed our tracking approach so users can log “route,” “site,” and “dose” alongside labs and symptoms, then share clear history with their clinicians rather than relying on memory.
Whether you stay with intramuscular injections or move to subcutaneous, consistent tracking helps you and your healthcare provider adjust intelligently instead of guessing.
Track Your TRT Protocol
Stop guessing. Start tracking. Your TRT protocol deserves better than spreadsheets.
Download HimculesRelated Reading:
Conclusion
Asking “Is subcutaneous or intramuscular better?” is a bit like asking whether a car or a bicycle is better—without saying what you need it for. For many chronic therapies, especially when patients self‑inject, subcutaneous administration often wins on comfort, convenience, and long‑term adherence, with equal or better outcomes in several drug classes.
At the same time, intramuscular injections remain essential for specific vaccines, some hormones, and situations where rapid, robust absorption is crucial or where the evidence strongly favors IM. From our standpoint, the best route is the one that matches the drug’s science, your medical needs, and your ability to stick with therapy over years, not weeks.
If you are considering a change from IM to SC (or vice versa), we encourage you to talk openly with your clinician, plan a monitoring strategy, and use tools like our Himcules tracking framework to see clearly how route changes affect your labs and how you feel. The more data and clarity you have, the easier it becomes to choose the route that is truly “better” for you.